BRAIN TRAINING
Neurofeedback for TBI’s
A wide range of injuries can occur in a car crash. Neck, back, and other musculoskeletal injuries are the most common, but one of the most commonly ignored or undetected injuries is a concussion or TBI. Mild TBIs are often not diagnosed after a car accident, sports injury, or slip and fall injury.
The diagnostic testing that is traditionally used to evaluate brain injury consists of imaging that looks at brain structure like CT, MRI, PET, or SPECT scans. While these tests can be pretty helpful, the results are often with in normal limits in patients suffering from traumatic brain injury because those diagnostic tests don’t tell us much about brain function.
The diagnostic testing we use in our offices to help evaluate traumatic brain injury is designed to measure brain function problems rather than structure. By assessing eye movements, balance, brain waves, memory, reaction time, sleep problems, and other parameters, we can better understand the ideal treatment options for patients suffering from a brain injury.
Check out the excessive head movement in these motor vehicle collisions that could cause a mTBI.
What is a Traumatic Brain Injury?
A traumatic brain injury (TBI) is a type of concussion. A TBI is caused by a blow to the head (focal TBI) or forceful shaking or rapid head movement (diffuse TBI), both of which can occur in a car accident. Even those involved in slow-speed car accidents can suffer from a mild TBI. A whiplash-type injury is when the head whips front to back (Head-on impact), back to front (Rear-end impact), or side to side (T-Bone impact). During a whiplash injury, sudden head movement may cause the brain to bounce back and forth against the skull, causing a minimal concussion or mild Traumatic Brain Injury (mTBI). Also known in the medical world as a contrecoup head injury.
In some cases, the victim may or may not lose consciousness. Regardless of consciousness, a traumatic brain injury could affect your memory, balance, coordination, and other essential brain functions.

How common are mTBI?
mTBI is a very common injury. When a person receives proper medical care after suffering an mTBI or concussion, there are usually no long-term effects. However, not receiving treatment can cause a person to suffer from lasting brain damage. The Centers for Disease Control (CDC) says that falls and car accidents are the two most common causes of brain injuries (including concussions) that resulted in hospitalization. Unfortunately, hospitals are not appropriately equipped with the necessary diagnostic tools to properly diagnose or treat an mTBI, and therefore often go undiagnosed.
When Should I Get Tested Or Evaluated For mTBI?
If you are involved in a motor vehicle collision, you should always seek medical care immediately. If you choose not to seek medical care, you could be putting your life or health at risk. Many people assume they are not injured because they feel no pain immediately after a crash, but this is often due to a release of adrenaline and other natural pain killers by our bodies when a crash occurs. A mTBI is frequently misdiagnosed, or worse, not diagnosed at all after a car crash. Hospitals do not have the necessary equipment to test for TBI. After a car crash, most injuries are neck and back-related, and orthopedic physicians often overlook the common TBI complaints. The damage that occurs to the brain during a traumatic event is immediate. Testing can be performed either within the first week of the accident, or years later. Once the damage or neuronal dysregualation occurs, it doesn’t get better on its own. A mTBI left untreated will manifest into further brain damage and may cause irreversible damage to the brain.
The Signs of a mTBI
Someone may suffer a mTBI and not even realize it. An mTBI or concussion left untreated can lead to long-term complications, such as chronic headaches, memory problems, vertigo, severe headaches, dizziness, mood swings, and brain fog that can last for months or years. Recent research and literature confirm that a mTBI can lead to the early onset of Dementia, Alzheimer’s, or other neurological-related deficits in severe cases.
The signs and symptoms of a mTBI may not display the same for every person. It is important to understand that adults and children may show signs differently. Many signs of a mTBI can be immediately apparent. However, some TBI symptoms may not appear for hours, days, weeks, or even months after a car crash.
The most common signs and symptoms of a car accident TBI include:
- Anxiety when driving or in a car
- Headaches, or pressure in the head
- Confusion or feeling “foggy.”
- Blurred or fuzzy vision in one or both eyes
- Mood swings – moody, irritable, sad
- Sleeping more or less than usual/trouble falling or staying asleep
- Difficulty concentrating or slowed thinking, Can’t seem to get your thoughts together.
- Lack of concentration and focus. When reading a book, you feel you have to read a sentence over and over again to understand it.
- Balance problems or coordination concerns
- Slurred speech
- Nausea and vomiting
- Loss of smell acuity – due to damage to the Olfactory Cranial Nerve
- Increased fatigue – Tired all the time despite getting enough sleep.
- Difficulty remembering new information
- Nauseous
- Day-to-Day Anxiety/panic attacks
- Dizziness, light headed, seeing floating stars
- Forgetfulness – Forgetting where you put things, forgetting details about a recent or past event.
- Lose your train of thought mid-sentence
Sometimes these symptoms may appear to get better on their own, but frequently the body learns to cope with the mental confusion, or the patient learns to live with it.
EVIDENCE-BASED DIAGNOSIS
Diagnosing a mTBI is very tedious and precise. At Hope Health & Wellness, we use state-of-the-art evidence-based protocols for diagnosing and treating Traumatic Brain Injury. Our team of physicians includes a board-certified neurologist, neuropsychologist, audiologist, psychologist, psychiatrist, and neuro-ophthalmologist.
Our goal is to help patients recover from the consequences of a TBI and improve their quality of life after suffering a traumatic brain injury.
WE USE SOPHISTICATED COMPUTERIZED TESTING TO DIAGNOSE AN MTBI
Quantitative Electroencephalogram Testing – (qEEG)
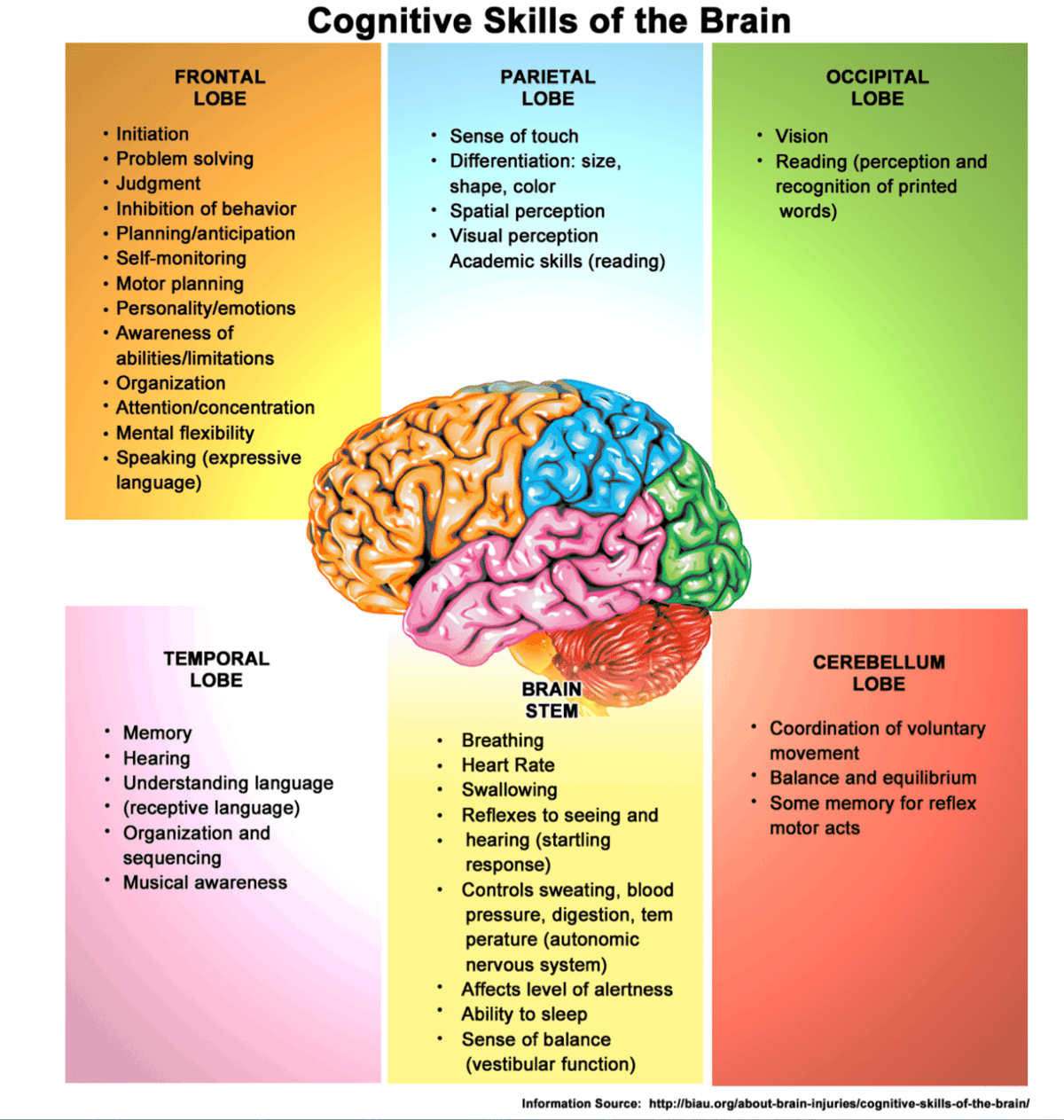
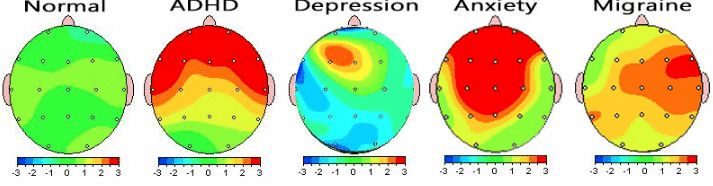
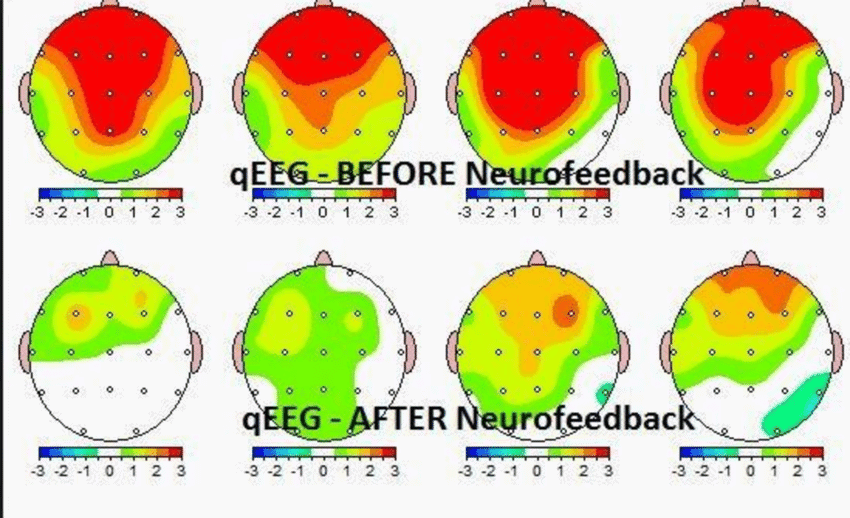
A qEEG (Quantitative Electroencephalogram) is a diagnostic tool that measures electrical activity and brain wave patterns and records the findings onto an image. This is often referred to as “brain mapping.” Brainwaves are the rhythmic electrical impulses generated when the billions of neurons inside the brain communicate with each other. Brainwaves can reveal necessary information about overall brain function, including stress levels, thought patterns, and emotions.
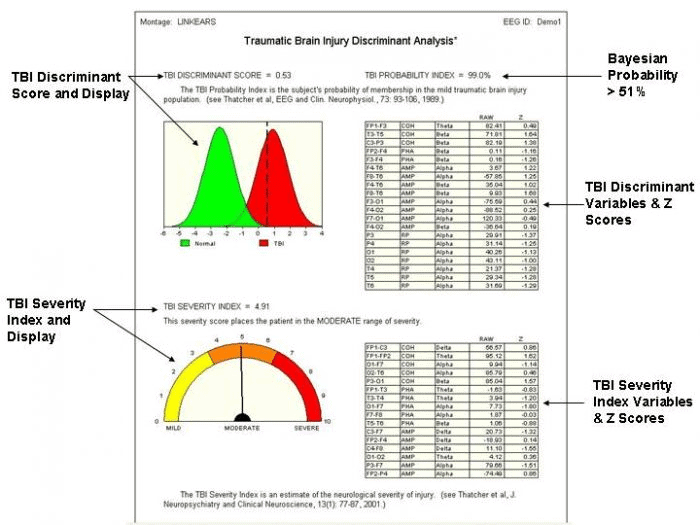
A qEEG helps to identify areas of the brain where any dysregulation may have occurred after an MVC or traumatic event resulting in a TBI. A qEEG evaluates a person’s brainwave patterns objectively and scientifically. Think of a qEEG Brain map like an EKG recording…it provides us with accurate information about the entire brain and where problems may lie.
A qEEG generates a recording of your brain’s electrical activity through tiny sensors at different parts of your brain.
After an MVC, we use a specific computerized qEEG TBI protocol with TBI biomarkers to record brainwave activity and determine the severity of the TBI (mild, moderate, severe). The results will pinpoint precisely where the TBI occurred in the brain, indicating the deficits that may present themselves.
A qEEG recording of your brain wave activity typically takes less than 30 minutes. We record your brain wave activity with your eyes open and closed, which provides enough raw data to formulate a diagnosis and determine where any dysregulation may occur in your brain.
We place you in a comfortable chair, it is essential that you relax as much as possible and limit your movement in the chair. Avoid excessive swallowing, and minimize any form of muscle tension as much as possible. It often helps to imagine and place yourself in the most relaxing frame of mind; as if you are on the beach or getting a massage.
The results are then analyzed to create a multi-color brain map, which we will review with you, in person, at your next appointment.

Oculomotor Tracking –
Eye Movement Tracking
Oculomotor tracking technology allows us to see what the eyes are following. This is of great importance because one of the most common symptoms of TBI is disrupted communication between the eyes and the brain.

Olfactory Testing
When the brain is injured, the sense of smell, known as olfactory function, is often altered. Many patients with TBI report alterations in their ability to smell or taste due to damage to the brain’s specific areas that control these functions. Our in-office olfactory testing allows us to assess any changes in these senses to better understand what areas of the brain have been affected.

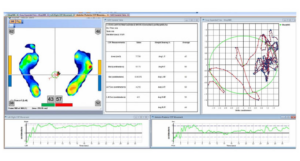
Computerized Balance Testing
Decreased balance and loss of coordination are some of the more commonly reported symptoms following traumatic brain injury. Studies show that between 30-65% of patients will report balance problems with TBI. Injury to the brain can affect communication with the inner ear and the eyes, creating a sensory mismatch that can lead to balance dysfunction, dizziness, or vertigo.
Computerized Neuro-Cognitive Assessment Test: (CNS)
This procedure utilizes scientifically validated, objective, and reliable computerized neuropsychological tests to evaluate the patient’s neurocognitive status. This computerized evaluation will cover a range of mental processes from simple motor performance, attention, memory, processing speed, and executive functions.
Computerized Adaptive Test
Mental Health Evaluation
All patients complete a computer adaptive mental health evaluation. The purpose of this test is to evaluate the level of depression, anxiety, PTSD, and other psychological conditions that may have manifested because of the accident.

Audiometry
It has been estimated that over 50% of individuals with traumatic brain injury may have an auditory processing disorder (Musiek et al 2004). Even minor head injuries can cause damage to the central auditory nervous system. However, imaging techniques and medical procedures may fail to detect the neural damage.

EVIDENCE-BASED TREATMENT
We use a technique called Electroencephalogram Neurofeedback Therapy (EEG – NFT).
Neurofeedback uses a sophisticated operant conditioning protocol, a learning method that employs positive and negative rewards. This is designed to retrain or reorganize brainwaves to help facilitate healing by utilizing visual and auditory stimuli. Our program is specific to traumatic brain injury and monitors brainwave function.
Neurofeedback encourages the neurons to communicate better, allowing for stronger neural synapses that can reduce and improve the common symptoms related to traumatic brain injury (mTBI).
This treatment aims to retrain and repair the dysregulated brainwave frequencies to allow better neuronal communication.
We typically recommend 12 neurofeedback sessions over six weeks followed by a repeat qEEG every 3 months to monitor progress and make necessary changes in treatment protocols for further treatment if needed. It’s not uncommon for some conditions to take months to years to reverse.
A follow-up qEEG and cognitive evaluation is performed to assess and document any improvement or impairment and the need for any additional treatment. Once we achieve the desired results and the qEEG reads more green patterns and less irregular brain wave patterns, the results are often permanent.
Our board-certified neurologist reviews all diagnostic testing and establishes a treatment protocol.
Why Hope Health & Wellness?
Highly Trained
Our commitment to providing the highest level of care by custom-designing your program to meet your specific needs and goals.
Cutting Edge Technology
We offer the most innovative technology and techniques in the field to get faster results for your recovery.
Pledge of Excellence
We aim to inspire “Hope” and enhance clinical education and research so that we can continue leading the industry with the latest treatment to ensure outstanding patient outcomes.
